The Management of Pancreatic Trauma in the Modern Era
Surgical Clinics of North America. Volume 87, Issue 6 (December 2007)
Diagnosis
- Grading system
- Serum amylase levels
- CT
- ERCP
- DSS MRCP
- Exploratory laparotomy
Pancreas Organ Injury Scale of the American Association for the Surgery of Trauma
Grade
|
Injury
|
Description
|
I
|
Hematoma
|
Minor contusion without duct injury
|
|
Laceration
|
Superficial laceration without duct injury
|
II
|
Hematoma
|
Major contusion without duct injury or tissue loss
|
|
Laceration
|
Major laceration without duct injury or tissue loss
|
III
|
Laceration
|
Distal transection or parenchymal injury with duct injury
|
IV
|
Laceration
|
Proximal transection or parenchymal injury involving ampulla
|
V
|
Laceration
|
Massive disruption of pancreatic head
|
CT findings suspicious for an injury to the pancreas include the following:
- hematoma surrounding the pancreas
- fluid in the lesser sac
- thickening of the left anterior Gerota's fascia.
CT scans can also demonstrate parenchymal lacerations or transections of the main pancreatic duct.
ERCP is the most reliable method to define continuity of the main pancreatic duct accurately.
Grade
|
Description
|
I
|
Normal main pancreatic duct on ERCP
|
IIa
|
Injury to branches of main pancreatic duct on ERCP with contrast extravasation inside the parenchyma
|
IIb
|
Injury to branches of main pancreatic duct on ERCP with contrast extravasation into the retroperitoneal space
|
IIIa
|
Injury to the main pancreatic duct on ERCP at the body or tail of the pancreas
|
IIIb
|
Injury to the main pancreatic duct on ERCP at the head the pancreas
|
Exploratory Laparotomy
In those patients who are taken emergently to the operating room for abdominal trauma, pancreatic injuries are diagnosed at exploration and it is important to establish the continuity of the main pancreatic duct.
Nonoperative Management
If there is no evidence of a ductal injury on fine-cut CT, non-operative management is acceptable, although it may be wise to perform ERCP to establish normal ductal anatomy definitively.
Operative Treatment
Indications
- Peritonitis on physical examination
- Hypotension and a positive FAST
- Evidence of disruption of the pancreatic duct on fine-cut CT or on ERCP
Isolated injuries to the pancreas without ductal involvement
General principles and exposure
During laparotomy, the initial priorities are control of active hemorrhage and control of gross gastrointestinal contamination.
Simple external drainage
In the hemodynamically stable patient, pancreatic contusions (AAST grade I), minor capsular injuries, and traumatic pancreatitis can be treated without drainage.
Most other injuries require drainage of some sort.
Treatment options for isolated pancreatic injuries based on the American Association for the Surgery of Trauma pancreas Organ Injury Scale
AAST grade
|
Treatment options
|
I
|
Observation
|
|
Omental pancreatorrhaphy with simple external drainage
|
II
|
Simple external drainage
|
|
Omental pancreatorrhaphy and drainage
|
III
|
Distal pancreatectomy ± splenectomy
|
|
Roux-en-Y distal pancreatojejunostomy
|
IV
|
Pancreatoduodenectomy
|
|
Roux-en-Y distal pancreatojejunostomy
|
|
Anterior Roux-en-Y pancreatojejunostomy
|
|
Endoscopically placed stent
|
|
Simple drainage in damage control situations
|
V
|
Pancreatoduodenectomy
|
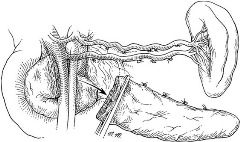
Isolated pancreatic injuries with ductal involvement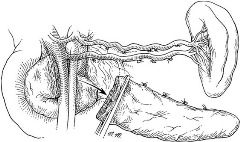 Distal pancreatectomy
Distal pancreatectomy
In the
hemodynamically stable patient with an isolated pancreatic injury, especially a child 10 years of age or younger, splenic salvage should be considered.

If the patient is
hemodynamically unstable, an expeditious distal pancreatectomy with splenectomyshould be performed.
 Roux-en-Y distal pancreatojejunostomy
Roux-en-Y distal pancreatojejunostomy is indicated in
hemodynamically stable patient who has a transection of the pancreas at the neck or just to the right of the mesenteric vessels and few associated injuries.
Combined pancreatoduodenal injuries
Pancreatoduodenectomy is indicated when there is extensive trauma to the head of the pancreas, a severe combined pancreatoduodenal injury, or destruction of the ampulla of Vater.
- In the hemodynamically stable patient, this procedure can be performed at the time of the original trauma laparotomy.
- In most of the patients who are hypothermic, acidotic, or coagulopathic, a damage control procedure is indicated. In this instance, the pancreatoduodenectomy or the reconstruction after a prior pancreatoduodenectomy should be performed at the reoperation.
- Control of hemorrhage and gastrointestinal contamination must occur first.